Breaking Down the Math on Reference-Based Pricing
If only all employers could be as innovative and hard-charging as ... the federal government? Oof.
The Committee for a Responsible Federal Budget (yeah, I’m as shocked as you that this exists. Must be the least popular group in all of D.C.) just dropped a detailed analysis on implementing RBP for the Federal Employee Health Benefits program. Buried in there is a roadmap for what ANY employer can expect when they stop letting hospitals yank them around with astronomical chargemaster pricing and just as phony carrier “discounts.”
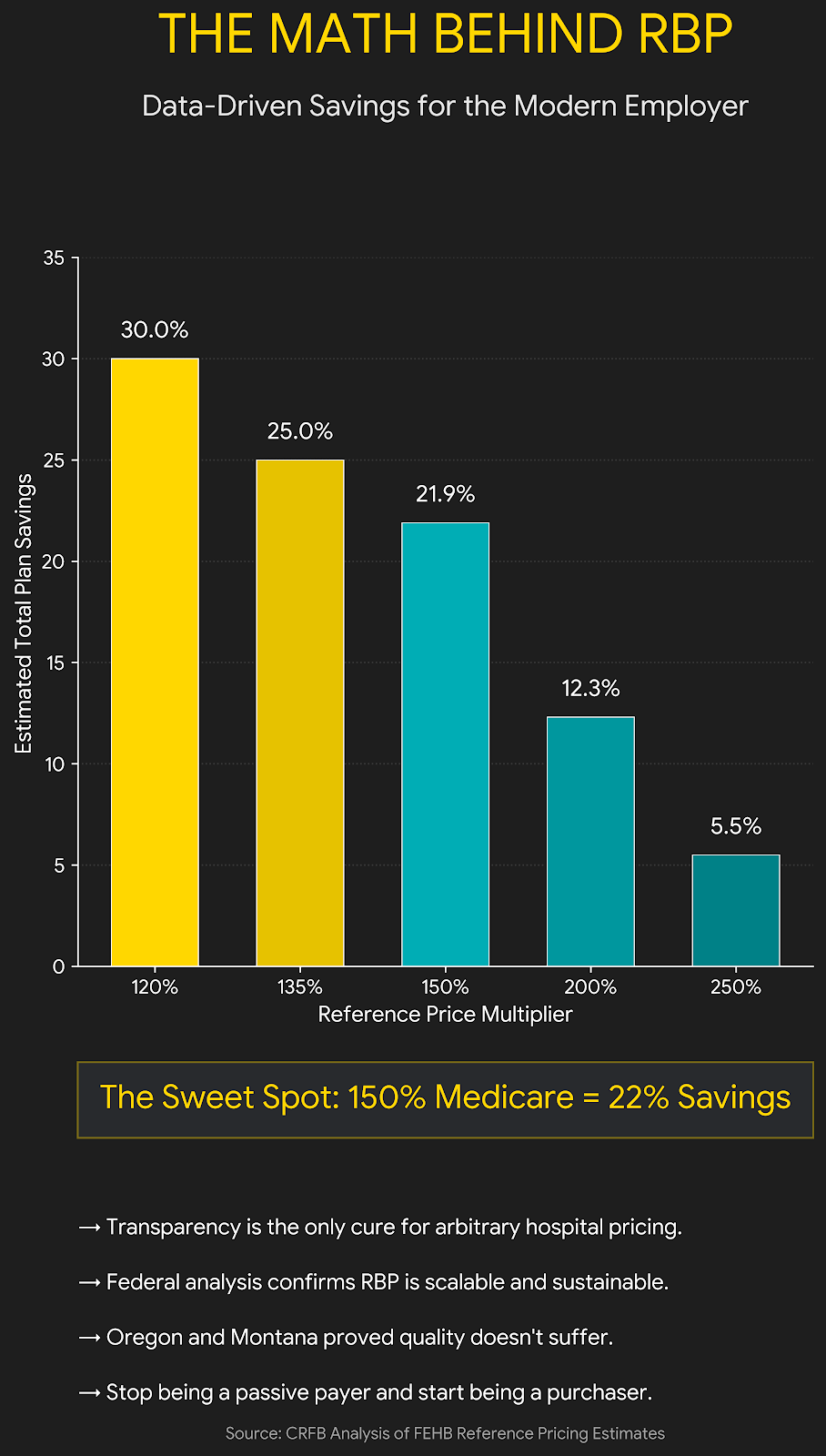
The government’s proposed pricing target amount of 200% of Medicare will deliver about 12% total savings. Go to 150% of Medicare? You’re looking at 22% savings. Even at 250%, you still get 5-6% back.
It’s not the first time that a governmental entity, you know, the ones known for their innovation, aggression, and hard-charging “move fast and break things” attitude, has done this. Oof. Even with a keyboard dipped in a vat of sarcasm, I couldn’t write that without a full-blown belly laugh. Had I written that in church, I’d almost certainly have spontaneously combusted.
Cali-Topia began doing this for select procedures in its government health plan back in 2011. Oregon’s done it. Montana did it. Washington state just enacted it, and they’re seeing substantial savings while simultaneously pushing hospitals to be less wasteful and more efficient.
What makes this particularly interesting for employers is that the FEHB program is basically a jumbo, nationwide employer plan. 8.2 million people. $73 billion in spending. Same dynamics you’re dealing with, except now we have actual data on what happens when you implement RBP at scale.
And the mechanics transfer directly. If you’re an employer paying 250-300% of Medicare right now (and you almost certainly are), you can model your savings pretty easily using this framework.
The objections are predictable: “But what about rural hospitals?” “What if providers leave the network?” “Won’t this hurt quality?”
Oregon exempted critical access hospitals. They set an out-of-network rate slightly lower to incentivize participation. And after implementation? No measurable impact on quality, access, or hospital financial stability. Once again, as we see over and over and over, the hospital apologist crowd silently puts on their big boy pants, tightens up the budget, and stops charging $74 for a band-aid or $49.99 for an ibuprofen.
I’ve attached a simple chart showing the correlation between the Medicare percentage you peg to and the savings you can expect. Use it to model your own scenarios.
The real question isn’t whether RBP works. We’re seeing it work all across America. It’s whether you’re willing to use your market power to actually do something about costs instead of paying tribute to the healthcare cartel with your employee compensation and company profitability.


Really smart breakdown of the RBP math. That line about hospitals tightening budgets and stopping $74 band-aids cuts right thru the fearmongering around quality concerns. Been watching similar dynamics play out in other sectors where established players inflate baseline costs, and the pattern is always the same once someone calls it out.