Becoming an HR Superhero, Prescription Drug Plunder & Stop Buying So Much Insurance
The Opaque Industry Secretly Inflating Prices for Prescription Drugs
I have a bit of a mash-up here in this post.
Enjoy!
The NYT has published a fantastic piece on the rampant waste, fraud, and abuse embedded in America’s prescription drug supply chain. The entire article is certainly worth your time. Below is a short synopsis of the full story.
The Opaque Industry Secretly Inflating Prices for Prescription Drugs
Pharmacy benefit managers are driving up drug costs for millions of people, employers, and the government.
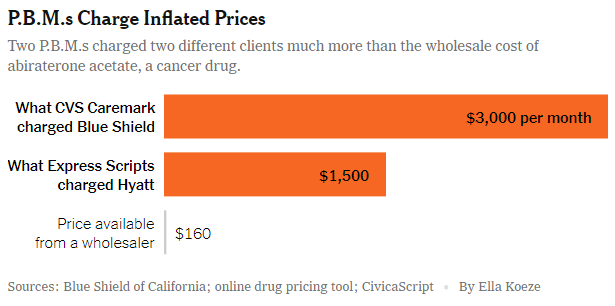
Pharmacy Benefit Managers (PBMs) are supposedly employed to reduce the costs of prescription drugs. However, a comprehensive investigation by the New York Times reveals that these managers frequently achieve the opposite effect. They have been found to direct patients toward more expensive medications, impose substantial markups on otherwise affordable drugs, and amass billions through concealed fees.
The largest PBMs, often prioritizing their financial interests over the needs of clients and patients, have been known to push patients toward drugs that carry higher out-of-pocket costs, while ignoring more cost-effective alternatives. This places a significant financial burden on patients, a fact that various state-specific examples highlight:
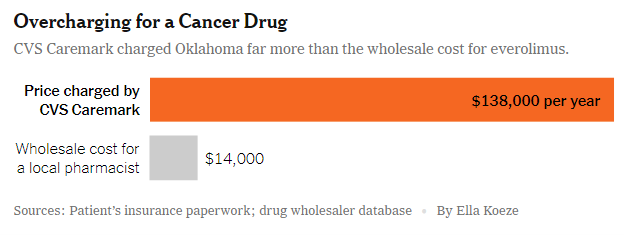
In Oklahoma, CVS's PBM, Caremark, reportedly overcharged the state employees' health plan by over $120,000 annually for a single patient's cancer treatment.
Similarly, in Illinois, a cancer patient ended up paying hundreds of dollars more for pain medication because Caremark mandated the use of a pricier drug variant.
In New Jersey, Express Scripts, a PBM owned by Cigna, told a 77-year-old retiree that his three-month supply of an allergy drug would cost $211, despite it being available for $22 at Costco.
The cumulative effect of these overcharges significantly contributes to the profitability and rapid growth of the PBM industry. Antonio Ciaccia, a consultant for Ohio and other states investigating these managers, criticized their role in the healthcare system, stating, “PBMs save money off bogus inflated prices that should not exist in the first place. They are the arsonist and firefighter of high drug prices.”
The tactics employed by PBMs have evolved over time, with a clear intent to continue reaping profits. PBMs and their new subsidiaries began imposing additional fees on drug manufacturers, distinct from traditional rebates. These fees are collected by separate entities, a deceptive practice that allows PBMs to claim they return most of the rebates to employers while omitting the disclosure of these fees.
Kent Rogers, a former executive at Optum Rx who contributed to the establishment of Emisar, explained that the intention behind creating a fee structure through Group Purchasing Organizations (GPOs) is to generate revenue that does not need to be passed on to clients. This enables PBMs to maintain a revenue stream essential for growth and pleasing stockholders.
One clear example of PBMs' reluctance to reduce costs is observed with Humira, a leading medication for arthritis. After two decades without generic competition, cheaper alternatives finally emerged in 2023. Despite potential annual savings of up to $6 billion for employers, insurers, and patients, PBMs were slow to make the switch. Data from IQVIA indicated that, as of March, 96% of prescriptions were still for the more expensive brand-name drug, primarily because Humira's manufacturer, AbbVie, paid substantial fees to the PBMs’ GPOs.



Once again thank you! Last year my prescriptions were 3 month supplies that I got at my local, small pharmacy. This year, unless I go with Optum RX, I can only get 1 month at a time. And last month, the insurance wouldn't allow a refill unless I called Optum RX to have them opt me out. (on the plus side the lady in customer service was very nice and it wasn't complicated to opt out). While these prescriptions total less than $5/month for me, I want to support my local, small town pharmacy even it if means going in once a month for refills.